1Department of Obstetrics & Gynaecology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh; 2Department of Gynaecological Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
 10.3329/bmrcb.v45i2.42539
10.3329/bmrcb.v45i2.42539  0000-0003-3471-5832
0000-0003-3471-5832
Background:Cervical cancer is the commonest cancer in women in developing countries. Visual inspection with acetic acid (VIA) is much popular method as primary screening modalities in low resource setting.Whereas Pap smear is well recognized and popular in developed countries. Colposcopy is recognized as the best method for detection of cervical cancer and cervical intraepithelial neoplasia (CIN) as secondary screening. The present study was intended to compare the accuracy of Pap smear and colposcopy in the detection of pre-invasive cervical lesion in VIA positive cases.
Methods: This cross sectional study was carried out in the Colposcopic Clinic of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka over a period of 1 year from August 2015. All consecutive VIA positive cases were included the study.
Results: Mean age of the VIA positive women was 36.9 years with peak age group being 31-40 years (44.0%). Nearly three-quarters of the women (74.0%) were in their 3rd and 4th decades of life. Among VIA positive women, 35.0% were Pap positive and 55.0% were colposcopically positive and 41.0% were histopathologically positive. Pap smear had low sensitivity (53.7%) and high specificity (78.0%). Using Pap smear nearly half (46.3%) of the precancerous lesion were escaped. Whereas colposcopy findings, revealed high sensitivity (90.2%) and specificity (69.5%). Both Pap and colposcopy was judged against histopathological diagnosis. Over 40.0% of the VIA positive women were diagnosed as CIN confirmed by histopathology. Strength of agreement test using Kappa statistics revealed a moderate agreement between Pap smear test and colposcopy (49.5%).
Conclusion: The study concluded that colposcopy has a high sensitivity, optimum specificity and moderate agreement against histopathology in relation to Pap smear. Pap smear has very little role whereas colposcopy has significant role for diagnosis of CIN. So, it would be adopted and encouraged to do the colposcopy where it is possible.
Keywords: Visual inspection with acetic acid (VIA), Colposcopy, Pap smear, Pre-cancerous lession
Cancer of the cervix is the second most common life-threatening cancer among women worldwide.1 New cancer cervix cases per year is 500,000 of which 79.0% occur in the developing countries, leading to cancer death 233,000 from the disease.2
Although widespread use of Pap test screening over the last 4 decades has led to marked reduction in the incidence and mortality, it is still a public health problem in the developing countries.3
Aetiological association and possible risk factors for cervical carcinoma have been extensively studied. The major risk factors for cervical cancer includes early age at first intercourse, multiple sexual partners, low socioeconomic status, HPV infection, cigarette smoking and extended use of oral contraceptives.2
Well-organized and applied public education and cytology screening as well as changes in socio-economic profile have led to declines in cervical squamous cell carcinoma (SCC) incidence and mortality rates worldwide. Higher percentage decline in SCC is observed in countries where organized screening programmes are available.4 In the low-income countries the incidence of the disease is still high because of lacking of well-organized screening programme.5,6
Among the economically underprivileged nations like Bangladesh the statistics regarding cervical cancer are really horrible. Every year 17,686 women are diagnosed with cervical cancer and 10364 women die from the disease.7 The important reasons for higher cervical cancer incidence in developing countries are lack of effective screening programmes and less well-organized health system due to lower health budget. In the low income countries like Bangladesh, 60-80% of cases are seen in advanced stages which may explain why cervical cancer is the leading cause of life lost in women in South Central Asia, Latin America, and sub-Saharan Africa.8
The persistence and severity of precancerous changes influences the progress of the disease. The likelihood of regression of CIN I, CIN II, CIN III is 60.0%, 40.0%, 33.0% respectively and progression to invasive stage is 1.0%, 5.0% and greater than 12.0% respectively. The time interval between infection and development of cervical cancer varies and is apparently more than 15 years.9
Apart from the risk factors that are already described, the most important risk factor in low income countries is infrequent cervical screening or lack of accessible cervical screening services. Infection with high-risk strain of human papilloma virus (HPV) are of the root causes of cervical cancer. The virus-cancer link works by triggering alterations in the cells of the cervix, which can lead to the development of cervical intraepithelial neoplasia (CIN), which may be turned into invasive cervical cancer (ICC) subsequently in women with multiple sexual partner.10
More than 150 types of HPV are acknowledged among them fifteen are high risk types. Type 16 and 18 are generally acknowledged to cause about 70% of cervical cancer.11
Colposcopy is the procedure where the cervix is visualized through optical instruments used to detect changes in the cellular pattern of covering epithelium and vascularity of the underlying tissue. Colposcopy is a clinical method of detection of cervical cancer and CIN. Colposcopic evaluation and guided biopsy remains a critical diagnostic step for women with squamous intraepithelial lesions to identify women who require treatment.
Thus, in the context of adopting VIA-based and Pap smear based approaches, as primary screening modalities in low resource settings. Colposcopy may then be used to identify women who are likely to benefit from immediate treatment. The study was aimed to colposcopic evaluation of Pap smear for the detection of cervical intraepithelial neoplasia against histopathology among all VIA positive cases. Furthermore, it was also designed to evaluate the rate of CIN and its grade according to Pap smear, colposcopy and histopathological diagnosis to determine the sensitivity and specificity of Pap smear in the detection of pre invasive cervical lesion, and also to observe the sensitivity and specificity of colposcopy and to find the strength of agreement of these diagnostic modalities.
This cross sectional analytic study was carried out in the Colposcopic Clinic of the Department of Obstetrics & Gynaecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka over a period of 1 year from August 2015 Data were collected after approval from Institutional Review Board (IRB). The women with positive VIA test attended at Colposcopy Clinic in the Obstetrics & Gynaecology Department, BSMMU, Dhaka were the study population.
Patients with current pregnancy, menstruating women or pervaginal bleeding, obvious growth of cervix suggestive of malignancy, diagnosed case of carcinoma cervix, those who were not interested to be included were exclude from the study.
The sample size was determined using the following formula.
n = (Z2 ⨯ p ⨯ q)/d2, where
Z = Standard normal deviation = 1.96
p = Anticipated sensitivity of “Pap smear” in correctly diagnosing and differentiating CIN = 80% = 0.80.
q = (1-p) = 20% = 0.20, and
d = Desired accuracy or degree of allowable error (here 10% of p)
Sample size, n = [1.962⨯ 0.8 ⨯ (1-0.8)] / (0.08)2 = 96.
So, at least 96 patients were required in addressing the research question and obtaining a statistically valid result. But in the study 100 patients were included. Purposive sampling technique was employed to include the required number of patients.
The main outcome variables studied were as follows:
Pap smear finding – presence of CIN
Colposcopic findings – presence of CIN and its grade
Histologic findings – presence of CIN and its grade
Pap’s smear |
Frequency (n) |
Percentage (%) |
|---|---|---|
ASCUS |
15 |
15.0 |
LSIL |
12 |
12.0 |
HSIL |
8 |
8.0 |
Chronic cervicitis |
65 |
65.0 |
Colposcopic findings |
||
CIN-I |
41 |
41.0 |
CIN-II |
11 |
11.0 |
CIN-III |
3 |
3.0 |
Chronic cervicitis |
45 |
45.0 |
Histopathologic findings |
||
CIN-I |
28 |
28.0 |
CIN-II |
9 |
9.0 |
CIN-III |
3 |
3.0 |
Microinvasion |
1 |
1.0 |
Normal/cervicitis |
59 |
59.0 |
Age of the study population were ranging from 21–60 years (Mean age=36.9±7.8). Total 100 VIA positive women were subjected to Pap smear followed by colposcopy and histopathology. The study was intended to determine the screening accuracy of Pap smear and colposcopy against the histopathological diagnosis.
Regarding their education over half 53.0% (n=53) were secondary, higher secondary leveland 26.0% (n=26) primary level. Almost all were married and majority 91.0% (n=91) were house-wife.
Majority 91.0% (n=91) of the patients were married at the age of 10 – 20 years. The mean age at first child birth was 18.5 years (range: 15 – 25 years). Ninety nine percent of the patients were multiparous. Ninety one patients had NVD and 8.0% had caesarean section.
About half (49.0%) of the patients were OCP user and 23.0% were DMPA user and 25 were users of other methods. Over one-quarter (26.0%) did not use any methods.
Pap test demonstrates that 15 cases were ASCUS, 12 LSIL, 8 HSIL and 65 were chronic cervicitis of the 100 VIA positive patients, CIN-I =41, CIN-II =11, CIN-III=3 and the rest 45 were chronic cervicitis. Histopathological findings show that CIN-I=28, CIN-II=9, CIN-III=3, micro invasion=1 and the rest 59 were normal/cervicitis.
Paps test |
Histopathologic Comment |
Total |
|
|---|---|---|---|
Positive |
Negative |
||
Positive |
22 |
13 |
35 |
Negative |
19 |
46 |
65 |
Total |
41 |
59 |
100 |
Colposcopic Comment |
Histopathologic Comment |
Total |
|
|---|---|---|---|
Positive |
Negative |
||
Positive |
37 |
18 |
55 |
Negative |
4 |
41 |
45 |
Total |
41 |
59 |
100 |
The accuracy or validity of Pap test in diagnosing CIN according to the formulae for computation of the components of accuracy the sensitivity of Pap test in correctly detecting CIN in those who had the disease is (22/41) × 100 = 53.7% and its specificity in correctly excluding those who did not have the disease is (46/59) × 100 = 78.0%. Likewise the positive and negative predictive values of the Pap test are (22/35) × 100 = 62.9% and (46/65) × 100 = 70.9% respectively. The percentages of false positive and false negatives are (13/35) ×100 = 37.1% and (19/65) ×100 = 29.2% respectively. The overall diagnostic accuracy was calculated to be (2 + 46)/100 = 68%.
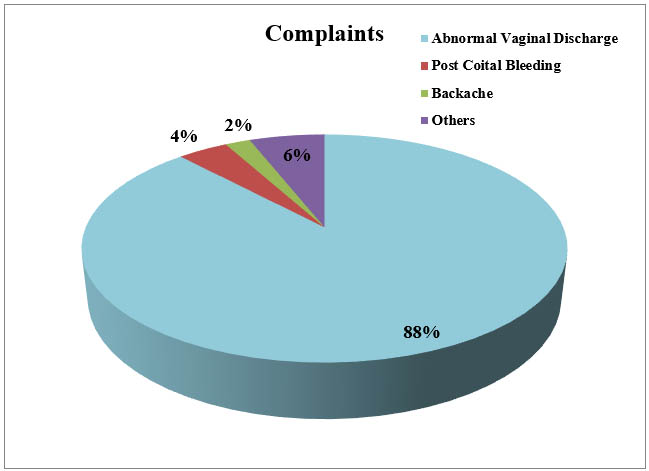
Figure 1: Distribution of patients by their complaints (symptoms)
Contraception: About half (49.0%) of the patients were OCP user and 23.0% were DMPA user and 25 were users of other methods. Over one-quarter (26.0%) did not use any methods (figure 2).
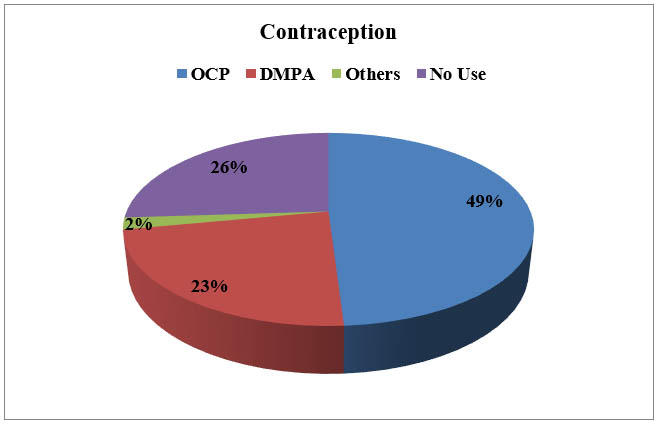
Figure 2: Distribution of patients by contraceptive use (n = 100)
Likewise using the formulae for computation of the components of accuracy, the sensitivity of colposcopy in correctly detecting CIN in those who had the disease is (37/41) × 100 = 90.2% and its specificity in correctly excluding those who did not have the disease is (41/59) × 100 = 69.5%. Likewise the positive and negative predictive values of the colposcopic diagnosis are (37/55) × 100 = 67.3% and (41/45) × 100 = 91.9% respectively. The percentages of false positive and false negatives are (18/55) ×100 = 32.7% and (4/45) × 100 = 8.9% respectively. The overall diagnostic accuracy was (37 + 41)/100 = 78.0%.
Strength of agreement between the two diagnostic modalities (Pap Test and colposcopy) was analyzed to see whether one screening test could be substituted for another cost-effective test. Accordingly moderate agreement was noted between Pap test and colposcopy (k = 0.495).
Disease studied |
Diagnostic modalities |
k value |
p value |
Strength of agreement |
|
|---|---|---|---|---|---|
CIN |
Paps Test |
Colposcopy |
0.495 |
<0.001 |
Moderate |
Invasive cervical cancer develops after a long phase of pre-cancerous lesion. The main aim of this study was to determine the accuracy of papsmear in comparison to colposcopy in the detection pre-invasive cervical lesion.
The mean age of the VIA positive women in present study was 36.9 years with peak age group being 31-40 years (44.0%) which matches with that of Jahan (35.7 ± 5 years) and Sankaranarayanan et al (38.9 ± 7 years).
Among all VIA positive women, only 35.0% were Pap positive, 55.0% were colposcopically positive and 41.0% were histopathologically positive. As histopathology is the gold standard for evaluation of cervicallesion the findings suggest that Pap smear has a low sensitivity (53.7%) but a high specificity (78.0%). Koutsky and colleagues demonstrated the sensitivity of Pap smear in detecting pre- cancerous cervical lesions is 51%.The sensitivity and specificity of the Pap test in detecting cervical intraepithelial neoplasia have been shown to be 55.4 and 96.8%, respectively. Colposcopy findings against histopathological diagnosis, revealed high sensitivity (90.2%) and optimum specificity (70.0%). So over 90.0% of the CIN positive women and 70.0% of the disease negative women screened out by colposcopic evaluation. As the colposcopy has both high sensitivity and optimum specificity, it can be considered as a better screening modality for early screening of CIN. As strength of agreement test using kappa statistics revealed a moderate agreement (57.0%) between colposcopy and histopathology and a fair agreement (32.3%) between Pap test and histopathology. So, colposcopy should be considered as a method of screening.
Colposcopy could not be employed in every setting for financial constraint. There is alternative of colposcopy is Gynocular which is battery operated and handy. Whereas Pap smear needed a lab setup, skilled person for conducting the procedure and also time consuming. If Gynocular is not available VIA could be an alternative to colposcopy. Present study showed 41.0% of the VIA positive women were histopathologically positive. Results of VIA and Colposcopy are available immediately which is reverse of Pap smear.
Results of VIA tests are available immediately, which reassures those who are test negative, and in test positive cases, it is possible to institute further diagnostic investigations like colposcopy to confirm the diagnosis, and a screen-and-treat approach, which offers treatment during the same visit. This is in contradistinction to Pap smear, in which the reporting of cytology test is not available immediately and is associated with recall for collection of investigation results and treatment, during which some of the clients may be lost to follow-up. Poor compliance with follow-up is a major obstacle to management of patients with abnormal cervical smears in resource poor countries.
Conclusion
The study concluded that colposcopy has a high sensitivity, optimum specificity and moderate agreement against histopathology in relation to Pap smear. Histopathologically proven nearly half of the patients were unidentified during screening by pap smear. Pap smear has very little role whereas colposcopy has significant role for diagnosis of CIN. So, it would be adopted and encouraged to do the colposcopy where it is possible. However, as colposcopy cannot be employed in every setting for financial limitations. Now a day’s handy colposcopy machine named Gynocular, available in all government medical colleges, where colposcopy is not possible, VIA may be used.
References
- Behtash N, Mehrdad N. Cervical cancer: screening and prevention’, Asian Pac J Cancer Prev, 2006; 7(4): 683-6. PMid: 17250453.
- Turkistanlı EC, Sogukpınar N, Saydam BK, Aydemir G. Cervical cancer prevention and early detection–the role of nurses and midwives. Asian Pacific Journal of Cancer Prevention. 2003; 4(1):15-21. PMid: 12718696.
- Achour M, Zeghal D. Cervical Cancer in Women with Inflammatory Pap Smears. Journal of Cancer Therapy. 2014 Jan 1; 5(1):82-90. DOI: 10.4236/jct.2014.51011
- Mathew A, George PS. Trends in incidence and mortality rates of squamous cell carcinoma and adenocarcinoma of cervix–worldwide. Asian Pac J Cancer Prev. 2009 Oct; 10(4):645-50. PMid: 19827887.
- Miller BA, editor. Racial/ethnic patterns of cancer in the United States: 1988-1992. DIANE Publishing; 1997.
- Howe SL, Delfino RJ, Taylor TH, Anton-Culver H. The risk of invasive cervical cancer among Hispanics: evidence for targeted preventive interventions. Preventive Medicine. 1998 Sep 1;27(5):674-80. https://doi.org/10.1006/pmed.1998.0343
- WHO. Human Papilloma Virus and Cervical Cancer (Summary Report), Bangladesh. Updated year 2013 (rl).
- Doh AS, Nkele NN, Achu P, Essimbi F, Essame O, Nkegoum B. Visual inspection with acetic acid and cytology as screening methods for cervical lesions in Cameroon. International journal of gynecology & obstetrics. 2005 May 1;89(2):167-73. https://doi.org/10.1016/j.ijgo.2004.12.040
- Ostör AG. Natural history of cervical intraepithelial neoplasia: a critical review. International journal of gynecological pathology: official journal of the International Society of Gynecological Pathologists. 1993 Apr;12(2):186-92. PMID:8463044
- Marrazzo JM, Koutsky LA, Kiviat NB, Kuypers JM, Stine K. Papanicolaou test screening and prevalence of genital human papillomavirus among women who have sex with women. American journal of public health. 2001 Jun;91(6):947-52. PMID: 11392939
- Wright Jr TC, Cox JT, Massad LS, Twiggs LB, Wilkinson EJ. 2001 consensus guidelines for the management of women with cervical cytological abnormalities. Jama. 2002 Apr 24;287(16):2120-9. doi:10.1001/jama.287.16.2120