Kawasaki disease (KD) is an acute self-limiting inflammatory disease associated with vasculities, affecting predominantly medium sized vessels and encountered these cases infrequently in clinical practice. The most concerning complication is coronary artery aneurysm (CAA) leading to myocardial infarction or sudden death. Fever is the essential feature. Kawasaki disease is invariably associated with an inflammatory process with elevated C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) and white blood cell count. Early recognition and treatment with IVIG (Intravenous venous immunoglobulin), and Aspirin showed highest protection against development of coronary artery disease. Incidence of KD is more in East Asia or in Asian ancestry living in other countries. The reason for high incidence in developing country is still unknown. Recently a significant number of cases attended in day to day practice which led conducting this study to assess the pattern of presentation, management and outcome after treatment and to aware the health care providers about the nature of the disease. This observational study conducted during September 2014 to March 2016. All the cases reported to the department of paediatric echocardiography for coronary artery analysis and suspected as KD were included in the study. History, clinical examination and investigation reports were analyzed from records. Age, gender, clinical feature, management, follow-up, echocardiography findings and outcome were analyzed. Data were collected from records of Echocardiography Department and Paediatric Cardiology Department of Lab Aid Cardiac Hospital and Combined Military Hospital, Dhaka. Among 27 cases, 16 were male (49.25%) and 11 were female (40.75%). Age distribution showed 8 (29.63%) were under one year of age, 13(48.14%) were in 1-5 years age group, 6 (22.23%) were in more than 5 years age group. All 27 cases were presented with fever, strawberry tongue, conjunctivitis, skin rash with peeling. Raised ESR, CRP and neutrophilic leukocytosis were found in all 27 cases. Cervical lymphadenopathy was found in 15 (55.52%) cases. Coronary artery changes were observed in 24 cases (88.89%). IVIG was given in 25 (92.60%) cases and Aspirin was given in 27 cases. Complete cure was achieved in 25 (92.59%) cases and one case died from thrombo-embolic event of radial artery and amputation of hand. The outcome of KD depends on the severity of coronary artery involvement. Patients with aneurysm larger than 08 mm are at highest risk of myocardial infarction. Less than 08 mm aneurismal dilatation regress with time. In this series outcome was excellent due to timely diagnosis and proper intervention.
Kawasaki disease is a syndrome composed of acute febrile illness of unknown cause which affects under five children.1,2 This disease was first described by Tomisaku Kawasaki in 1967.1 Incidence is high in Asian and Pacific region which is 30 per 100,0002. There is seasonal predominance in winter and spring, and children less than one year of age are more prone to KD.3 KD is associated with systemic vasculitis particularly affecting the coronary arteries, causing coronary artery aneurysm in 15 to 25% of untreated patient. Two to three of untreated cases die from coronary vasculitis.3-5
In the United States, Kawasaki disease is considered as the leading cause of acquired heart disease in children5. Kawasaki disease develops quickly and runs an aggressive course over a period of weeks. Typically, the condition then resolves. Even though it resolves, there may be cardiac complications years later. Principal symptoms associated with Kawasaki disease include: spiking fevers that last 5 or more days (required to make a diagnosis of Kawasaki disease), inflamed conjunctiva (eyes) without pus, red chapped lips, red mucous membranes in the mouth, red tongue that has the appearance of a strawberry, rashes on the trunk of the body, red palms of hands and red soles of feet, edema of hands and feet, peeling skin on hands, feet and genitals, swollen lymph node usually near the neck and occasionally joint pain and swelling often on both sides of body.1-6During the acute illness, blood vessels throughout the body become inflamed. This vasculitis can produce several acute cardiac problems, including tachycardia; inflammation of the cardiac muscle (myocarditis), which in some cases can lead to severe, life-threatening heart failure and mild mitral regurgitation.7
Some suspect there is an infectious cause of Kawasaki disease, but none has been proven. There are several immunologic irregularities linked with Kawasaki disease, and some believe it is an autoimmune condition. In the United States, Kawasaki disease affects 4,000 children each year. It is more prevalent in Japan with occurrence of 5,000 to 6,000 cases each year 6,7.
After completion of diagnosis, treatment should be started immediately, so that damage to coronary arteries and heart can be prevented. Intravenous immunoglobulin (IVIG) given in high doses is considered standard treatment for Kawasaki disease. High-dose aspirin is typically a part of the treatment plan as well. With early treatment for Kawasaki disease, full recovery is possible for most, but 2% of Kawasaki disease patients die from complications of coronary artery inflammation. Echocardiography of the patient should be performed at 6 months interval at least for years after complete cure to exclude remote possibility of involvement of coronary arteries. Electrocardiography (ECG) is also advised in some centers.6 Cardiac enzymes are advised in case of thrombotic events in coronary arteries and myocardial infarction.3
As expert echocardiography for recognition of coronary artery involvement was available in Paediatric Echocardiography Department of Lab Aid Cardiac Hospital and Paediatric Cardiology Department of Combined Military Hospital, most of the suspected cases were referred in these two places for echocardiography. Furthermore, management needs involvement of pediatric cardiologist also. So, a large number of patients were attended from many centres mainly for diagnostic purpose by echocardiography, and later also for management.
Considering these, this study was designed to assess the clinical presentation, management and outcomes of management in two tertiary care hospitals in Bangladesh.
This was a descriptive cross-sectional study done over a period of one year from July 2012. The health managers responsible for mid level public health management were the study population. All Civil Surgeons (64), 372 Upazilla Health and Family Planning Officers (UHFPO), 221 Upazilla Family Planning Officers (UFPO) and 21 Program me Managers (PM) and Deputy Program me Managers (DPM) of different government programs and non-government organizations were mailed a structured questionnaire. The questionnaire included questions based on competency measuring scale developed by Janet Place, North Carolina Public Health Academy under University of North Carolina and modified by Public Health Foundation. 4 The scale comprises eight domains. Seventy-six competencies (indicators) under those domains cumulate the “core competencies”. The score obtained by the respondents were summed up and average score was calculated in each domain. The level of proficiency was scored 1 for “none”, 2 for “aware”, 3 for “knowledgeable” and 4 for “proficient”. Scale “none” is for if the respondent feel a need for improvement or 4 if s/he thinks that is excelling at that competency. Respondents were reminded by phone calls and e-mails several times. The overall response rate was 178/678 (26%). Finally resonses of 13 civil surgeons, 14 program managers and deputy program me smanagers, 113 upazilla health and family planning officers and 38 upazilla family planning officers were included in the analysis. Descriptive statistics, independent sample t test and correlations were done. Ethical approval was obtained from the Ethical Review Committee of National Institute of Preventive and Social Medicine (NIPSOM), Dhaka.
Eight (29.62%) cases were under one year, 13(48.14%) cases were between one to 5 years and 6 (22.23%) cases were above five years. Sixteen (49.25%) cases were male and 11(40.75) cases were female (table I).
Age |
Number |
Percentage (%) |
Less than 1 Years |
08 |
29.63 |
One to five Years |
13 |
48.14 |
More than 5 Years |
06 |
22.23 |
Sex |
|
|
Male |
16 |
49.25 |
Female |
11 |
40.75 |
All 27(100%) cases had fever, straw berry tongue, conjunctival congestion and peeling of skin. Cervical lymphadenopathy was observed in 15(55.56%) cases. Thrombocytosis was observed in 25(85.18%) cases. Raised CRP, ESR and neutrophilic leukocytosis were observed in all cases (table II).
Clinical/ Lab Findings |
Number |
Percentage (%) |
Fever |
27 |
100 |
Rash |
27 |
100 |
Peeling of skin |
27 |
100 |
Conjunctival congestion |
27 |
100 |
Cervical Lymphadenopathy |
15 |
55.55 |
Strawberry tongue |
27 |
100 |
Thrombocytosis |
25 |
92.59 |
Raised CRP and ESR |
27 |
100 |
Neutrophilic leucocytosis |
27 |
100 |
Aneurismal dilation of LCA (5 mm-8 mm) was noticed in 10(37.03%) cases, Dilated LCA (3mm-5mm) in 5(18.52%) cases, dilated RCA (3mm - 5mm) in 5(18.52%) cases, dilatation of both RCA and LCA was observed in 4(14.81%) cases and no coronary changes in 3(11.12%) cases. Heart failure was observed in 2(7.41%) cases and pericardial effusion was observed in 1(3.70%) case (table III).
Disease |
Number |
Percentage (%) |
LCA aneurysmal change(Z score >2.5 to <5 and <8 mm) |
10 |
37.03 |
Dilated LCA (Z score 2 to <2.5) |
05 |
18.51 |
Dilated RCA (Z score 2 to <2.5) |
05 |
18.51 |
Dilated LCA+ RCA Change |
04 |
14.81 |
No Change (Z score <2) |
03 |
11.11 |
Heart Failure |
02 |
7.4 |
Pericardial effusion |
01 |
3.70 |
Twenty-five (92.60%) cases received IVIG and all 27 cases received aspirin in high dose initially followed by low dose. Corticosteroid was not used in any cases (table IV).
Disease |
Number |
Percentage (%) |
IVIG in single dose 2 gm/kg over 10 hours |
25 |
92.59% |
Aspirin in high doses (100mg/kg) |
27 |
100% |
Aspirin in Low doses (5mg/kg) |
27 |
100% |
Corticosteroid |
NIL |
00% |
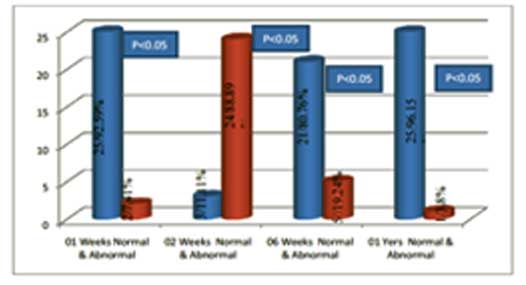
At 1st week 25 (92.59%) cases had normal echo findings. At 2nd weeks 24 (88.89%) cases had abnormal echo. At 6 weeks 21(80.76%) cases had normal Echo and at one year 25 (96.15%) cases had normal echo and 1(3.80%) case had abnormal echo (figure 1).
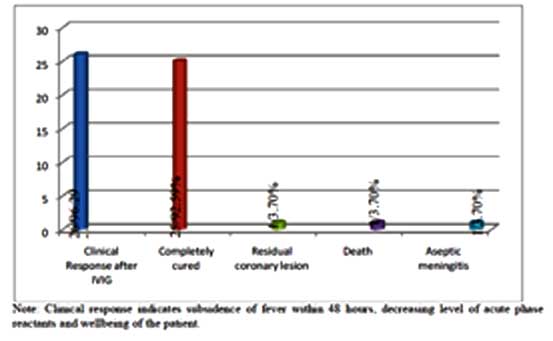
At 1syear follow up twenty five cases were found completely cured, only one case had slightly dilated left coronary artery (p <0.05). Death due to thrombotic complication of radial artery was one in acute stage (figure 2).
Kawasaki disease is the commonest cause of acquired heart diseases in children. It is the 2nd commonest vasculities illness of childhood after Henoch Schonlein Purpura.4-8 Approximately 85% children with KD are under 5 years of age with peak incidence between 18 to 24 months. 1,8 In this study, most of the patients (48.14%) were in one to five years age group. Kawasaki disease is rare in less than three months or more than five years of age but coronary artery aneurysm is very common in this group.8 Thought there is ethnic bias towards Asian children but no study was conducted in Bangladesh to see the incidence. 7,8 Male preponderance noticed in all studies which corresponded with this study.5,6 There was seasonal preponderance also and it was found most of the cases reported between Septembers to March in this study.5 Kawasaki disease case numbers were highest in January through March and approximately 40% higher than in the months of lowest case numbers from August through October in northern hemisphere.6 The aetiology of KD is unknown but history of preceding respiratory tract infection and gastroenteritis was observed in 13 cases in this study. Many published report implicate a number of bacterial and viral pathogens including retro virus, Epstein bar virus, corona virus, staphylococcus, streptococcus as infectious triggers of KD. 7-10 Some studies support super antigen triggered process but others have not confirmed. Some studies suggest genetic contribution. These genes are ITPKC, ABCC4, FCGR2A, CD4D and a gene region near FAMI67A- BLK. Some genes are also associated with non-response to Immunoglobulin and coronary artery change including CASP3 and FCGR3B. 11-16
Diagnostic criteria for KD are fever for 5 days or more along with any four of the following features.3,4:
- Bilateral conjunctival congestion;
- Oral changes;
- Peripheral extremity changes;
- Rash; or
- Cervical Lymphadenopathy.
If coronary artery is dilated or aneurismal dilatation is present then only three clinical features are required for diagnosis. In this series fever, rash, oral changes, and conjunctival congestion was present in 100% cases. Coronary changes were noticed in 89.89% cases. Some of the cases are incomplete cases who have insufficient clinical features but they appear subsequently and coronary changes are very frequent in these cases.3 No incomplete cases in this series. Some KD cases may have aseptic meningitis, arthritis, pneumonitis, dysuria or otitis media. One aseptic meningitis case was found in this series. In measles predominant area, diagnosis of KD is sometime missed because of some similar features.6 As KD is invariably associated with inflammation, elevation of ESR, CRP, and raised WBC count is always there.4 In the absence of inflammation KD diagnosis is unlikely. Thrombocytosis appears towards the end of 2nd week, therefore may not be helpful.5 In this series, thrombocytosis was to be found in 92.59% cases. Echocardiography was done at diagnosis, at 2 weeks, at 6 weeks to look for coronary artery changes. Significant aneurysm more than 8 mm was not observed in any cases. Other cardiac complications like heart failure, arrhythmia, pericardial effusion, myocardial ischemia may occur in KD cases. 7 Most of the cases had dilated coronary arteries and treated with IVIG before developing aneurysm in this series. Intravenous immunoglobulin and Aspirin is the main drug used for treatment of KD.6 High dose aspirin was used in all cases. High dose aspirin of 100 mg/kg was given to patient till they became afebrile followed by low dose aspirin 5mg/kg till coronary arteries returned to normal. Early recognition and treatment with IVIG and aspirin can prevent coronary artery aneurysm which was shown by many studies.1,2,5,6 This study also supports this observation, and given IVIG to 25 cases but two cases came after 2 weeks of onset of illness when IVIG had no role in preventing coronary artery changes. Exact mechanism of action of IVIG is unknown, but it has generalized anti inflammatory property. Two gm/kg IVIG may be given as single dose. Randomized control trial comparing divided low dose IVIG (400 mg/kg/days for 4 days) versus a single infusion of high dose (2gm/kg over 10 hour) showed single dose infusion has a greater therapeutic effect in the prevention of CAA. 17,18 Single dose protocol was used in this series. Some studies showed corticosteroids were used in IVIG resistant cases to prevent coronary artery changes in 20% cases. But some other studies suggested that corticosteroids were associated with increased risk of CAA.19 No corticosteroid was used in any of cases. Clinical trials evaluating the use of corticosteroid plus IVIG have confusing results. But corticosteroids have some roles in (a) IVIG resistant cases, (b) patient with most severe disease, and (c) patient with coronary and peripheral aneurysm with confusing inflammation. 20-23 Prognosis of the disease depends on coronary artery involvement. As per American Heart Association, a new classification of coronary artery abnormalities is based on z-scores as follows:24,25
- No involvement: always <2
- Dilation only: 2 to <2.5, a decrease in Z score during follow-up ≥1
- Small aneurysm: ≥2.5 to <5
- Medium aneurysm: ≥5 to <10, and absolute dimension <8 mm
- Large or giant aneurysm: ≥10, or absolute dimension ≥8 mm.
IVIG should be administered as soon as possible within 10 days of fever onset.
Latest AHA guidelines highlight other situations in which IVIG may also be appropriate for patients who are beyond the 10-day window, and it is recommended for children who present after the 10th day with “ongoing systemic inflammation as manifested by elevation of ESR or CRP (CRP >3.0 mg/dL) together with either persistent fever without other explanation or coronary artery aneurysms (luminal dimension Z score >2.5).”
Patient with aneurysm more than 8 mm has greater risk of MI. Less than 8 mm aneurysm usually regresses in course of time. In this series aneurysm more than 8 mm was not observed in any cases. So outcome in these cases were excellent. One case who died, having radial artery thrombosis, and died from amputation related complications. One case had slightly dilated coronary artery up to one year follow-up.
Kawasaki disease (KD) is a self-limiting disease and usually resolves within 12 days, if there is no coronary or cardiac involvement. High dose aspirin should be stopped when patient become afebrile. Low dose aspirin should be continued until coronary become normal. CAA more than 8mm needs lifelong aspirin therapy. Echocardiography should be repeated at 2 weeks and 6 weeks for all cases and 6 monthly for those having CAA or dilated coronary arteries. In this series, outcomes were excellent, as standard guidelines were followed and only one patient died in acute phase, and was due to thromboembolic manifestation in radial artery and its surgical management, and not related to KD directly. KD should be included in differential diagnosis for any child suffering from unexplained fever with positive supportive findings.
References
- Harnden A, Alves B, Sheikh A. Rising incidence of Kawasaki disease in England: analysis of hospital admission data. BMJ. 2002;324:1424–25.
- Dillon MJ, Eleftheriou D, Brogan PA. Medium-size-vessel vasculitis. Pediatr Nephrol. 2010;25:1641–52.
- NewburgerJW, Takahashi M,Gerber MA. Diagnosis, treatment, and longterm management of Kawasaki disease. Circulation. 2004; 110:2747–71.
- Brogan PA, Bose A, Burgner D. Kawasaki disease: an evidence based approach to diagnosis, treatment, and proposals for future research. Arch Dis Child. 2002; 86:286–90.
- MacNeil A, Holman R, Yorita K. Evaluation of seasonal patterns of KawasakiSyndrome-and rotavirus-associated hospitalizations in California and New York, 2000–2005. BMC Pediatrics. 2009; 9:65
- Chang, FengYu. Characteristics of Kawasaki disease in infants younger than six months of age. The pediatric infectious disease journal 2006; 25 :241-44.
- Cai Z, Zuo R, Liu Y. Characteristics of Kawasakie disease in older children. Clin Pediatr (Phila). 2011;50;952.
- Meissner HC, Leung DY. Superantigens, conventional antigens and the etiology of Kawasaki syndrome. Pediatr Infect Dis. 2000;19:91.
- Gardner-Medwin JM, Dolezalova P, Cummins C. Incidence of Henoch-Schonlein purpura, Kawasaki disease, and rare vasculitis in children of different ethnic origins. Lancet 2002;360:1197–202.
- Brogan PA, Shah V, Clarke LA. T cell activation profiles in Kawasakisyndrome. Clin Experim Immun. 2008; 151:267–74.
- Holman RC, Christensen KY, Belay ED. Racial/Ethnic Differences in the Incidence of Kawasaki Syndrome among Children in Hawaii. Hawaii Medical Journal. 2010;69:194.
- Fujita Y, Nakamura Y, Sakata K. Kawasaki disease in families. Pediatrics.1989; 84:666–9.
- Weng KP, Hsieh KS, Hwang YT. IL-10 polymorphisms are associated with coronary artery lesions in acute stage of Kawasaki disease. Circ Journ. 2010; 74:983.
- Dominguez SR, Anderson MS, El. Adawy M, Glode MP. Preventing coronary artery abnormalities: a need for earlier diagnosis and treatment of kawasakiedisease. Pediatr Infect Dis J. 2012; 31:1217
- Weng KP, Ho TY, ChiaoYH. Cytokine genetic polymorphisms andsusceptibility to Kawasaki disease in Taiwanese children. Circ Journ. 2010; 74:2726.
- Onouchi Y. Molecular genetics of Kawasaki disease. Pediatr Res. 2009;65:46R–54R.
- Onouchi Y. Genetics of kawasaki disease. Circul J. 2012; 76:1581.
- Burgner D, Davila S, Breunis WB. A genome-wide association study identifies novel and functionally related susceptibility Loci for Kawasaki disease. PLoS Genetics. 2009;5:e1000319.
- Kobayashi T, Inoue Y, Takeuchi K. Prediction of intravenous immunoglobulin unresponsiveness in patients with Kawasaki disease. Circulation. 2006;113:2606–12
- TremouletAH, Best BM, Song S. Resistance to intravenous immunoglobulin in children with Kawasaki disease. J Pediatr.2008;153:117–21.
- Furukawa T, Kishiro M, Akimoto K. Effects of steroid pulse therapy onimmunoglobulin-resistant Kawasaki disease. Arch Dis Child. 2008; 93:142–6.
- Bourusly M, Jawad N. Case report: Kawasakie disease in A Kuwaiti family. Kuwaiti Medical Journal 2005;37:110-12.
- Anderson DG, Warner G, Barlow E. Kawasaki disease associated with streptococcal infection within a family. J Paediatr Child Health 1995; 31:355–7.
- Sundel R. Initial treatment and prognosis of Kawasaki disease [monograph on the Internet]. [cited 2008 Nov 4]. Available from:www.utdol.com/patients/content/topic.do?topicKey=~zn7eQ5L/HSALoa.
- Newburger JW, Takahashi M, Gerber MA. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Circulation. 2004; 110:2747-71.
- Mc Crindle BW, Rowley AH, Newburger JW et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association [published online March 29, 2017]. Circulation.doi:10.1161/CIR.0000000000000484
- American Heart Association. Kawasaki Disease. http://www.heart.org/ HEARTORG/ Conditions/More/ Cardiovascular Conditionsof Childhood/Kawasaki-Disease_UCM_308777_ Article. jsp#. WRMzdFXytaS. Accessed May 9, 2017. Last reviewed May 2017.