Pott’s disease is a common cause of neurological complications and kyphotic deformity.When deformity progressed that may lead to painful costo-pelvic impingement, respiratory distress, risk of paralysis of muscle of lower limb and consequent reduction in quality andlongevity oflife. The treatmentstrategy is to avoid neurological complication and achieve a near normal spine. In tuberculosis, spinal column may become unstable. Pathological fracture or dislocation of a diseased vertebral body may occur due to mechanical insult. Surgical decompression causefurther instability.The insertion of a metallic implant is to provide stability. Pedicle screw fixation in kyphotic correction in old Pott’s disease is a most suitable device.This prospective interventionalstudywas conducted in BanglabandhuSheikh Mujib Medical University (BSMMU) for aperiod of 60 monthsfrom July 2011, with at leasttwo years follow-up period. Twentycases (13 males and 7 females) of thoracolumbar spinal tuberculosis with neurological deficit were operated with a transpedicular decompression and screw fixation along with anti-tubercular drug treatment. All of these patients had varying degrees of neurological deficit and single level involvement with vertebral body destruction and mild kyphosis of 9–28 degrees. Long segment pedicle screw fixation, posterior decompression, and correction of kyphosis were performed in single stage.The mean age of patients was 50.9 and kyphosis improved from 17.85±1.37 degrees to 10.85±2.66 degrees (p=0.0206).Neurological recovery occurred in 18 patients (90%). Bony fusion was achieved in 67.5% cases. At 2-years follow-up mean visual analogue score (VAS) score improved from 5.5 to 0.75 (p=0.0031).So, posterior decompression and transpedicular stabilization with continued chemotherapy is a good treatment option for the management of the thoracic and thoracolumbar TB in patients with vertebral body destruction and <30degree kyphosis.
Keywords: Transpedicular decompression, Pott’s paraplegia, Spinal tuberculosis, Kyphosis
Spinal tuberculosis (TB) is the most common form of extrapulmonary TB.1Like other TB, anti-tubercular chemotherapy is the mainstay of treatment for spinal tuberculosis. About 15–50% of spinal TB patients develop the most dreaded complication, that is, paraplegia.2Patients who are treated conservatively, though collapse may progress still bony fusion was noticed causing residual kyphosisup to 60 degrees.3 Therefore, surgery is indicated for the patient who developed neurological complication and persistent severe kyphosis. It is also indicated in acute onset, severe grade paraplegia, pain dueto instability, or in elderly patients.4Surgery improves neurological status by removal of compressive elements, that is pus, granulation tissue, sequestrum, and disk material. It also increases the vascularity, improves thedelivery ofdrug intodisease site, and thus helps in healing and bony fusion.5,6Though there is controversy about ideal surgical treatment.Decompression surgeries only with prolonged immobilization increased kyphosis.7-9As Pott’s being an anterior disease of vertebra, anterior decompression and fixation has been considered as the gold standard. But it has problems of anaesthetic complications, higher morbidities, peroperativevascular injury,graft failure, and poor fixations in ostaeopenicbone.10Sometimes even additional incision or surgery is required for posterior fixation.11 Hence, recently the posterior approach surgery has gained popularity, based on the principle of adequate but not extensive debridement and stable fixation, with much lower complication rates.4This prospective study was undertaken to evaluate the efficacy of posteriordecompression and fixation in thoracic and thoracolumbar TB with definite surgical indication in skeletally mature patients.
The prospective interventional study was conducted among 20 patients (13 males and 7 females) during July 2011 to June 2016 at BSMMU and Popular Hospital, Dhaka. Themean age of the study population was 50.9 years with a range of 32–71years. Cases available during the study period were included following inclusion and exclusion criteria. Patients with thoracic or thoracolumbar spinal TB involving two adjacentvertebrae with neurological deficits and destruction of the vertebral bodies, kyphotic angle less than 30 degree were included in the study. Furthermore, those having Frankel grade A/B paraplegia,Frankel C/D paraplegia not responding to chemotherapy within four weeks, and/or those with severe pain with VAS score more than five also included.
Patients with medical co-morbidity, advance stage of spine TB,more than one level paravertebral involvement, multifocal lesion andkyphotic angle>30 degree were excluded from the study.All the cases were confirmed by CT guidedFNAC. Haemtological workup CBC,LFT done before starting 4-drug oral antitubercular chemotherapy regimen (isoniazid 5-10mg/kg/d, rifampicin 10-20mg/kg/d, ethambutol 15-25 mg/kg/d, and pyrazinamide 25-35 mg/kg/d) for three months followed by isoniazid and rifampicin for 15 to 18 months.Surgical procedure:The patient was positioned prone with onebolster beneath chest and other below pelvis so that the abdomen could hang free. This position may help in reducing some amount of kyphosis due to gravitational pull. With midline incision and stripping of the paravertebral muscles, the pedicle screws were inserted in the unaffected vertebrae (above and below the diseased site). The affected segments were avoided as there was a previous report of loosening of the screw with subsequent subcutaneous abscess formation. After placement of pedicle screws, decompression was performed at the extradural compression in the MRI picture. The pedicle of the vertebra in which the body is more eroded and destroyed, was usually selected for removal. With the help of power burrs, the inferior facet of the adjacent superior vertebra was excised first and then the upper facet and pedicle were removed until body of the vertebra. For better visibility, small part of the adjoining lamina was also cut; although majority of laminar parts were preserved.The existing nerve root would be visible now.With retraction of the nerve root, the compressive elements, that is, granulation tissues, sequestrated bone and discwere removed, preferably with angled curettes and discforceps protecting the spinal cord .The tissue was sent for histopathologic examination. Paravertebral abscesses were also drained and sent for culture and sensitivity tests. In patient with involvement of L1–L2, adequate space was available for decompression through intervertebral foramen after partial removal of the facets from one side without removal of pedicle. Lastly, the connecting rods were fixed with pedicle screws on both sides after proper contouring.
Postoperative management:Sutures were removed after 14th postoperative day. Patients were mobilized 6 days after surgery with brace and advised to continue it for6 months and discharged the patient 10 days after surgery. ATT was continued for 15 to 18 months. Patients were followed up at 3 weeks then 3, 6, 12, 18 and 24 months. Neurological status was evaluated using the Frankel grading, pain was assessed using VAS, the angle of kyphosis was calculated from X-rays by Konstam and Blesovsky technique.
Of the total 20 cases,the mean age of the patients was 50.9 years. The mean vertebral body destruction was 0.51VBL. The mean follow-up period was 30.8 months.There was significant relief of pain (p=0.0031) in all patients with improvement of VAS using paired t-test for preoperative and final follow-up for 3 different levels.Relief of pain was assessed by visual analogue score.12Neurological status was evaluated by Frankel grading.13Erythrocyte Sedimentation Rate (ESR) of all the patients which was between 37 and 86 mm and preoperativelyreached to normal12 months after surgery. Eighteen (90%) out of 20 patients showed signs of neurological recovery. Elevenpatients (55%) recovered neurologically to Frankel grade E,two patients were in grade D, six in grade C, and three in grade B. Nine patients who showed neurological recovery to Frankel grade D, preoperatively four ofthem were in grade A and fivein grade B.
S.No |
Age (years)/sex |
Level of Involvement |
Pre-op Frankel’s grading |
Post-op Frankel’s grading |
Final Frankel’s grading |
Pre-op |
Post-op |
Final |
Pre-op kyphotic angle |
Post- op kyphotic angle |
Degree of correction |
Kyphotic angle at final FU |
Loss of correction at final |
Fusion |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
53/f |
T10-11 |
B |
D |
D |
7 |
3 |
1 |
20 |
17 |
3 |
17 |
0 |
Y |
2 |
67/m |
T12-L1 |
C |
D |
E |
6 |
2 |
1 |
9 |
3 |
6 |
3 |
0 |
N |
3 |
71/m |
T7-8 |
B |
C |
D |
7 |
3 |
1 |
27 |
12 |
15 |
14 |
2 |
Y |
4 |
53/m |
T8-9 |
A |
D |
D |
6 |
2 |
0 |
15 |
5 |
10 |
7 |
2 |
N |
5 |
41/f |
T3-4 |
B |
D |
D |
8 |
5 |
5 |
17 |
12 |
5 |
13 |
1 |
N |
6 |
47/m |
L1 |
D |
E |
E |
7 |
0 |
0 |
27 |
14 |
13 |
15 |
1 |
Y |
7 |
46/f |
T11-12 |
B |
D |
D |
6 |
3 |
0 |
19 |
12 |
7 |
14 |
2 |
Y |
8 |
57/m |
T3-4 |
C |
D |
E |
7 |
2 |
0 |
20 |
14 |
6 |
15 |
1 |
N |
9 |
43/f |
T5-6 |
B |
D |
E |
3 |
1 |
0 |
18 |
11 |
7 |
12 |
1 |
Y |
10 |
52/m |
T6-7 |
B |
D |
E |
6 |
3 |
1 |
27 |
18 |
9 |
21 |
3 |
N |
11 |
32/m |
T8-9 |
A |
C |
D |
3 |
1 |
0 |
21 |
15 |
6 |
16 |
1 |
Y |
12 |
31/m |
T10-11 |
B |
D |
D |
5 |
2 |
0 |
21 |
14 |
7 |
16 |
2 |
Y |
13 |
66/f |
T9-10 |
A |
C |
D |
5 |
1 |
2 |
15 |
3 |
12 |
5 |
2 |
N |
14 |
57/m |
T11-12 |
C |
D |
E |
6 |
2 |
1 |
18 |
9 |
9 |
10 |
1 |
Y |
15 |
48/m |
T7-8 |
C |
D |
E |
4 |
0 |
0 |
14 |
9 |
5 |
10 |
1 |
N |
16 |
59/m |
L1-2 |
D |
E |
E |
5 |
2 |
1 |
8 |
1 |
7 |
2 |
1 |
Y |
17 |
39/f |
T8-9 |
B |
D |
E |
4 |
1 |
0 |
12 |
10 |
2 |
10 |
0 |
Y |
18 |
51/m |
T9-10 |
A |
C |
D |
5 |
1 |
1 |
11 |
4 |
7 |
5 |
1 |
N |
19 |
48/f |
T11-12 |
C |
D |
E |
4 |
1 |
1 |
18 |
8 |
10 |
10 |
2 |
Y |
20 |
57/m |
T3-4 |
C |
D |
E |
6 |
0 |
0 |
20 |
14 |
6 |
15 |
1 |
N |
F= fusion; fix= fixation levels; FU= follow-up; L= lumbar; N= no fusion Y= fusion seen.
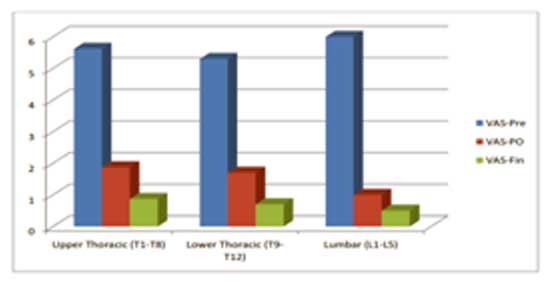
Figure 1: Preoperative, Postoperative and Final VAS score at different spinal levels.
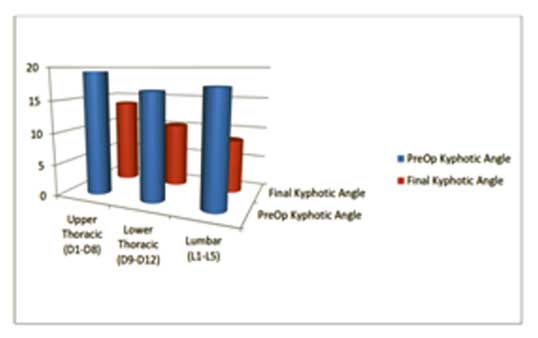
Figure 2:Kyhphotic angle: Preoperative and Final follow-up
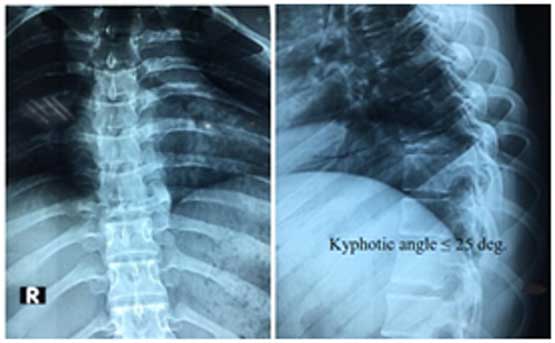
Figure 3: Preoperative X-ray AP and lateral view shows involvement of D6 vertebral body (central or body type of tuberculosis)

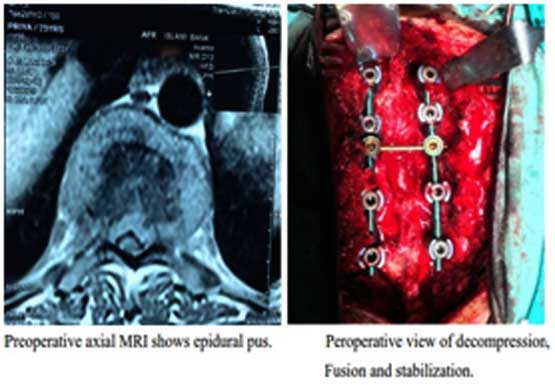
Figure 4: Preoperative MRI saggital section T1 and T2 weighted image showing involvement of D6 vertebral body with prevertebral and epidural pus.
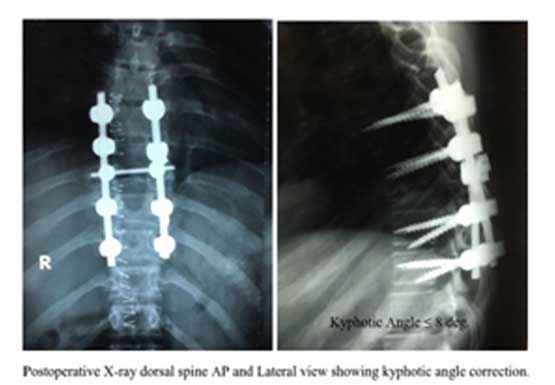
In final follow-up, 11 patients (55%) had radiologic fusion.Preoperative mean kyphotic angle 17.85±1.37 with postoperative 10.85±2.66. Kyphotic angle correction was statistically significant (p= 0.0206) using paired t-test.Bed sore was the most common complication, which occurred in three patients. Four patients (20 %) had urinary tract infection.
In reference to Frankel et al, Frankel grading was done as Grade A: Complete paralysis;Grade B: Sensory function only below the injury level;Grade C: Incomplete motor function below injury level;Grade D: Fair to good motor function below injury level;andGrade E: Normal function.13
For decompression of Pott’s disease, anterior approach is ideal, as the disease involve mainly anterior part of the body and disc. As the patientswereundernourished its very difficult to achieve satisfactory outcome by invasive approach like transplural.2Posterior approach with instrumentation were established as safe technique in treatment of Pott’s disease.4 Lee and colleagues have compared the result of transpedicular decompression to anterior decompression with fixations.4 All of their patients had complete neurological recovery and significant VAS improvement, but most of their neurological deficits (Frankel D or E) were less severe. In the present study, severe neurological involvement (Frankel grade A and B) was seen in 12 patients,of which all recovered to grade D or E. In the present study, the kyphosis correction was comparable with other posterior surgery series (5.16–9.6 degrees).4Furthermore, fusion was observed in only 55.5% cases despite adequate period of follow-up, but the patients without fusion had neither any pain nor any radiologic evidences of implant loosening at their latest follow-up. Previous study showed fusion upto100%.4 Though, rate of fusion is less,still transpedicular approach is usefultechnique for decompression and fixation of Pott’s patient with a very low complication rate.
There weresome limitations of thisstudyincluding limited sample size,variations in the level and neurological involvement. Furthermore, the exact time of onset of the disease was not known.
Based on the findings of the study, itmaybe concluded that transpedicular decompression and long segment stabilization with pedicle screw and rod is a good surgical option with less surgical risks for the treatment of thoracic and thoracolumbar tuberculosisin patients with bone destruction less than 50%.
Authors gratefully acknowledge the support of the Department of OrthopaedicSurgery, BSMMU and Popular Hospital,Dhaka to conduct the study.
References
- Pu X, Zhou Q et al. A posterior versus anterior surgical approach in combination with debridement, interbody autografting and instrumentation for thoracic and lumbar TB. 2012;36:307-13.
- Jain AK, Dhami IK. Tuberculosis of the spine, a review. ClinOrthop. 2007; 460:34-49.
- Jain AK. Fresh look at an old disease.J Bone Joint Surg. 2010;92:905-13.
- Lee TC, Lu K, Yang LC,Huang HY,Liang CL, Transpedicular instrumentation as an adjunct in the treatment of thoracolumbar and lumbar spine tuberculosis with early stage bone destruction. J Neurosurg (Spine). 1999;91:163-69.
- Jutte PC, Loenhout-Rooyackers JH. Routine surgery in addition to chemotherapy for treating spinal tuberculosis.Cochrane Database Syst Rev. 2006.
- Ge Z, Wang Z, Wei M. Measurement of the concentration of three antituberculosis drugs in the focus of spinal tuberculosis. Eur Spine J.2008;17:1482–87.
- Chacko A, Moorthy RK, Chandy MJ. The transpedicular approach in the management of thoracic spine tuberculosis: a short-term follow up study. Spine. 2004; 29:363-67.
- Upadhyay SS, Sell P, Saji J.Surgical management of spinal tuberculosis in adults Hong Kong operation compared with debridement surgery for short and long term outcome of deformity.ClinOrthop. 1994; 302:173-82.
- Jain AK, Aggarwal A, Dhammi IK.Extrapleural anterolateral decompression in tuberculosis of the dorsal spine. J Bone Joint Surg. 2004;86:1027-31.
- Hodgson AR, Stock FE.Anterior spine fusion for the treatment of tuberculosis of the spine. The operative findings and results of treatment in the first one hundred cases. J. Bone and Joint Surg 1960; 42:295-310
- Talu U,Gogus A, Ozturk C, Hamzaoglu A, Domanic U.The role of posterior instrumentation and fusion after anterior radical debridement and fusion in the surgical treatment of spinal tuberculosis: experience of 127 cases. J Spinal DisordTech.200619:554-59
- Guyatt GH, Townsend M, Berman LB, Keller JL. A comparison of Likert and visual analogue scales for measuring change in function. J Chronic Dis 1987;40:1129-33.
- Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 1969;7:179-92.