Abstract
Keywords: Gentamicin; Once daily dose; Neonatal sepsis; Trough concentration
Neonatal sepsis is one of the most common causes of neonatal morbidity and mortality in the preterm population.1Neonatal sepsis is a clinical syndrome characterized by signs and symptoms of infection with or without accompanying bacteremia in the first month of life. It encompasses various systemic infections of the newborn such as septicemia, meningitis, pneumonia, arthritis, osteomylitis and urinary tract infections.2 The World Health Organization (WHO) estimates that 1 million deaths per year (10% of all under-five mortality) are due to neonatal sepsis and 42% of these deaths occur in the first week of life. Neonatal sepsis accounts for approximately 23% of the world′s neonatal deaths, in developing countries 30-50% of neonatal deaths due to neonatal sepsis.3-5 Treatment of neonates with suspected sepsis should commence as soon as appropriate cultures and intravenous access can be obtained. The initial choice of antimicrobial agents for empirical treatment is dependent on the knowledge of the probable pathogens based on the perinatal history, including any maternal symptoms, cultures, or instrumentation and susceptibility pattern of the organisms. Based on the common antibiotic susceptibilities of the predominant organism causing early onset sepsis (EOS), the recommended initial empiric therapy for a neonate with suspected bacterial sepsis includes ampicillin and an aminoglycoside.6-9 This combination expands the antimicrobial spectrum and also offers synergistic bacterial killing. A drawback in the use of amino glycosides is their narrow therapeutic range and the potential nephrotoxicity and Ototoxicity.7,10-15 There is also large inter individual variability in gentamicin concentration in the neonate requires that its optimal dosing be defined.16-20 Generally accepted peak concentration is 5-10 microgram/ml. It has been suggested that even higher peak levels (e.g. 25 microgram/ml) do not increase the associated toxicity.21 It is also suggested that the trough concentration should be less than 2 microgram/ml to minimize the potential toxic effect. This study aimed to asses peak and trough concentration of gentamicin, and to asses renal function by measuring serum concentration of creatinine and ototoxicity by doing Otoacoustic emission (OAE).
This open label clinical trial was conducted in the Neonatal Intensive Care Unit (NICU), Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, during the period of March, 2012 to November, 2012. It was aimed to observe the peak (the efficacy) and trough concentration (toxicity level) of gentamicin in once daily dose (ODD) versus twice daily dose (TDD) as a primary outcome, and also to observe the renal and hearing status as secondary outcome in the neonates, treated with gentamicin. Peak level of gentamicin is the maximum concentration within 30 minutes to one hour after injection and expected concentration is to be 5 to 10 microgram /ml and trough level is the concentration of gentamicin that is measured before giving the next doe it must be <2 microgram/ml. Two groups were matched with the gestational age, post natal age and birth weight. Fifty neonates were enrolled in the study. After matching, lottery method was used to select the patient, lottery was conducted by duty doctor, this procedure continued till desired sample size was achieved informed written consent was taken before enrollment. Finally, 25 neonates were in ODD group and 25 in TDD group of gentamicin. All these neonates were diagnosed as suspected or culture proven sepsis and were treated with gentamicin and ampicillin. Neonates with post natal age 0- ≤28days and gestational age ≥32 weeks were included in the study. Newborns with perinatal asphyxia required resuscitation, gross congenital anomalies, renal impairment due to any cause were excluded. Suspected sepsis with presence of at least two risk factors of sepsis, which leaded to commence antibiotics (as per unit protocol for starting antibiotics) and proven sepsis was defined by the presence organism in blood culture or other body fluid or tissue culture. Patien′s demographic information were gathered including gestational age, birth weight, length, post natal age and weight at the time of therapy, maternal and baby′s risk factors for sepsis were also collected. Baseline investigations for sepsis were sent before commencement of treatment along with baseline serum creatinine was also done. Gentamicin was given, in ODD group 5mg/kg and in TDD group 2.5mg/kg 12 hourly. Both groups were concomitantly treated with ampicillin 50mg/kg 12 hourly.The required dose, was given as a one minute bolus into existing intravenous lines, followed by a flush with 0.5 ml normal saline. Serum trough gentamicin concentration was obtained before 3rd dose for ODD group and before 5th dose of TDD group. Peak concentration was collected one hour after gentamicin injection. At the same time, blood were collected for CBC, CRP, IT, PBF and for blood culture sensitivity and for serum creatinine. One ml of blood was collected through butterfly needle for analysis of peak and trough level of gentamicin. Peak and trough concentration was measured in the Biochemistry Department of the Bangabandhu Sheikh Mujib Medical University, to observe the primary outcome. Serum creatinine level was measured twice, once at admission and 2nd one at discharge, to observe renal function (as secondary outcome) and creatinine level raise of 50% from the baseline was define as renal function impairment.
Hearing test was done by otoacuastic emission test (OAE) at the ENT Department at discharge of the patient and hearing impairment was defined, if fails to pass OAE. Ethical approval was taken from the Institutional Review Board. SPSS software (version 19) was used for data analysis. Chi square test for comparison of demographic variable and qualitative data; unpaired t test for comparison of serum gentamicin concentration and paired t test was performed to compare serum creatinine. Duration of treatment was continued as per protocol of NICU.
Demographic data, age and sex, gestational age were comparable in both groups. Baseline clinical features and baseline investigations and culture positivity of the organisms were also comparable (table I).
Variables |
ODD Group |
TDD Group |
p value |
Age |
19(76) |
21(84%) |
0.47 |
Sex |
15(40) |
17(68) |
0.33 |
Gestational age |
40% |
40% |
0.93 |
Clinical Features |
80% |
84% |
0.99 |
Baseline lab. Features WBC |
15(60) |
16(40) |
0.46 |
Serum peak concentrations of gentamicin were 7.19±1.7 micrograms/ml in ODD and 4.81±1.8 micrograms/ml in TDD group which was significantly higher (p=0.001) in ODD group (table II).
Variable |
Once daily dose(ODD) |
Twice daily dose(TDD) |
p value |
Peak concentration |
7.19±1.7 |
4.814±1.8 |
0.001 |
Trough concentration |
1.5±0.78 |
2.00±0.90 |
0.04 |
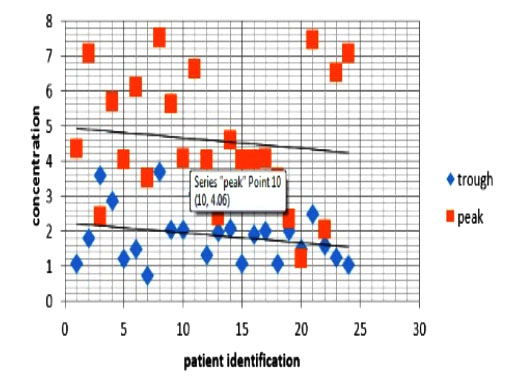
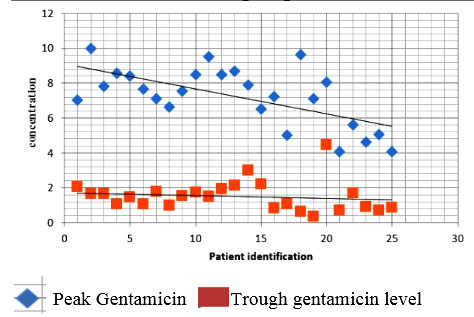
On the other hand, trough concentrations were 1.5±0.78 micrograms/ml in ODD group and 2.0±0.9 micrograms/ml in TDD group, and the difference was not statistically significant (p=0.04) (table II). Twenty (80%) patient in ODD group and 11 (44%) patient in TDD group reached the expected peak concentration (5-10 microgram/ml). On the other hand, 2 patients (8%) patient in ODD group and 6(24%) patient in TDD group crossed the toxic trough level ≥2microgram/ml (figure1 and figure 2).
Patients serum concentration of creatinine in ODD group was 0.532±0.146mg/dl at baseline and 0.568±0.106 mg/dl at discharge, and in TDD group, it was 0.532±0.151mg/dl at baseline and 0.556±0.112 mg/dl at discharge.
The differences were not statistically significant (table III). But, 2(4%) patients in TDD group had 50% raised in creatinine from the baseline but no patient in ODD group had such raised creatinine.
Variables |
Serum creatinine (mg/dl) |
|
At admission |
At discharge |
|
ODD group |
0.568±0.106 |
0.532±0.131 |
TDD group |
0.532±0.146 |
0.55±0.11 |
|
(p 0.29) |
(p 0.59) |
During discharge AOE was done, and only 4% patient in ODD group and 8% in TDD group has ototoxicity (Refer, means screening positive by OAE) it was non-significant statistically (table IV), but it was not followed-up for further assessment of hearing on subsequent visit.
OAE |
ODD |
TDD |
p value |
Pass |
24(96) |
23(92) |
0.55 |
Refer |
1(4) |
2(8) |
Discussion
A total of 50 newborns were included with suspected or culture positive sepsis. The number of male babies was higher than the female (male: female = 1.8: 1), which was consistent with other study.22 In this study, the peak concentration of gentamicin was significantly higher (p < 0.001) in once-daily group (7.19±1.7) microgram/dl compared to twice daily group (4.81±1.8). In addition, the peak concentration of gentamicin in ODD group remained significantly higher than the TDD group Several studies also reported higher peak concentration of gentamicin in ODD group.23 However, in one study reported no difference in peak concentration between ODD and TDD groups.24 In this study, no difference was to be found in serum concentration creatinine in between the groups rather tough concentration of gentamicin was higher in the twice daily dose group. This study had several strengths; the first strength was its design: Patients were allocated to each of the two treatment groups alternately, i.e. the first eligible patient was assigned to one study group then the next eligible patient was assigned to the other group. This sequence was followed until obtaining the total samples. As a result, the demographic and clinical characteristics of patients at enrollment were distributed evenly between the two treatment groups. The treatment effects those were observed the mean peak concentration of gentamicin was higher and the mean trough concentration was lower in the once-daily dose group is likely to be real. The second strength was that the outcomes were determined from biochemical analysis; hence, one of the objectives, assessment of the outcome had a high-level of accuracy. Furthermore, the study assessment included covariates, such as weight and gestational age, which were potentially strong confounders of the assessed relationship of dose and bioavailability of gentamicin. In contrast, limitations of the study included, firstly, sample size of the study was small; secondly, the assessment of sepsis clearance was under powered. Only a fraction of patients had sepsis at the time of enrollment. Although, more patients in the once-daily dose group had have sepsis clearance than the patients in the twice-daily dose group. The absolute number in each group was very small. Hence, the chi-square estimates were not likely to be valid. Thirdly, the study duration was short. The study did not include any long-term follow-up on patient′s vital status. For example, patients died after the study ended.
Conclusion
It may be concluded that therapeutic peak level (efficacy) of gentamicin is significantly higher in once daily group of gentamicin and trough level (toxic level) is also lower in this group. There was no significant renal and hearing impairment in any group.
References
- Polin RA, Richard A. Management of neonates with suspected or proven early-onset bacterial sepsis. Pediatrics 2012; 1291006-15.
- Gotoff SP. Infection of Neonatal Infant.In: Nelson Textbook of Pediatrics, Behrman RE, Kligman RM, Jenson HB (Eds). WB Saunders, Philadelphia. 2000, pp 538-552.
- Bang AT, Paul VK, Reddy HM, Baitule SB. Why do neonates die in rural Gadchiroli, India? (Part I): primary causes of death assigned by neonatologist based on prospectively observed records. Journal of Perinatology.2005; 25 :29-34.
- Vergnano s, Sharland M, Kazembe P, Mwansambo C. Neonatal sepsis: an international perspective. Arch Dis Child Fetal Neonatal Ed. 2005;90: F220-F224.
- Bang AJ, Bang RA, Baitule B. Burden of morbidities and unmet need for healthcare in rural India neonates: a prospective observational study in Gadchiroli, India. Indian Pediatr. 2001; 38:952-65.
- Grades JS. Clinicopathologic approach to the diagnosis of neonatal sepsis .Clin Perinatal.1991;18:361-381.
- Gudmundsson A, Erlendsdottir H, Gottfredsson M, Gudmundsson S. Impact of pH and cationic supplementation on in vitro post antibiotic effect. Antimicrob Agents Chemother. 1991;35: 2617-24.
- Gudmundsson A, Einarsson, S, Erlendsdottir H, Moffat J, Bayer W, Craig WA. The post antibiotic effect of antimicrobial combinations in a neutropenic murine thigh infection model. J Antimicrob Chemother. 1993; 31(suppl D):177-91
- Airede AI. Neonatal septicaemia in an African city of high altitude. J Trop Pediatr. 1992; 38: 189-91.
- Anaiz A .Pulse Dosing of Amino glycosides: A Consensus Document. International J.Clin Pharmacology & Therap. 2000; 35:22,3-226.
- Andronikou S,Giapros VI,Cholevas VI ,Popadopoulou ZL .Effect of aminoglycosides therapy on renal function in full terminfants. Pediatr Nephrol 1996; 10:766-68.
- Baltimore RS. Neonatal Sepsis: epidemiology and Management. Pediatric Drugs. 2000;5:723-740.
- Barza M, Ioanidis JPA, Cappelleri JC, Lau J. Single or multiple daily doses of aminoglycosides - a meta-analysis. BMJ. 1996; 312:338-345 .
- Bastone EB,Shu CL,Ioannides-Demos LL,Spicer WJ, McLean AJ. Kill kinetics and regrowth patterns of Escherichia coli exposed to gentamicin concentration-time profiles simulating in vivo bolus and infusion dosing. Antimicob Agents Chemother. 1997: 37:914-7.
- Barclay ML, Begg EJ,Chambers ST. Adaptive resistance following single doses of gentamicin in an in vitro dynamic model . Antimicrob Agents Chemothep.1999; 36:1951-7.
- Buckler B. Bell J, Sarn R. Unnecessary work up of asymptomatic neonates in era of group B streptococcus prophylaxis. Infect Dis obstet Gynecol. 2010 ;3:13-15.
- Blaser J, Stone BB,Groner M, ZinnerSH. Comparative study with enoxacin and netilmicin in a pharmacokinetic model to 9determine importance of ratio of antibiotic peak concentration to MIC for bactericidal activity and emergence of resistance. Antimicrob Agents Chemother. 1999; 31: 1054-60
- Boyle EM, BrookesI, Nye K, Watkinson M, Riordan FAI. Randon gentamicin concentrations do not predict trough levels in neonates receiving once-daily fixed dose regimens. BMC Pediatrics. 2006; 6: 1-7.
- Buckler B, Bell J ,Sarn R.Unnecessary work up of asymptomatic neonates in era of group B streptococcus prophylaxis. Infect Dis obstetGynecol. 2010; 3:13-15.
- Chambers HF. The Amino glycosides In: Brunton LL, Lazo JS,Parker KL, Eds. Goodman & Gilman's the pharmacologic basis of therapeutics. 11th Ed. McGraw Hill, 2006, pp 1155-71.
- Chambers, Chambers HF. The aminoglycosides. In: Goodman and Gillman's: The pharmacological basis of therapeutics. McGraw-Hill Publications, 2001; pp 3536.
- Chattopaday B. Newborn and gentamicin-How much and how often. Journal of antimicrobial chemotherapy. 2002; 49: 13-6.
- Skopnik H, Wallraf R, Nies B,Troster K, Heiman G. Pharmacokinetics and antibacterial activity of daily gentamicin. Arch Dis Child. 1992 ; 67:57-61.
- Solomon R, Kuruvilla KA, Job V. Randomized controlled trial of once vs. twice daily gentamicin therapy in newborn. Indian Pediatr. 1999; 36: 133-37.