Keyword: Platelet parameters,Acute coronary syndrome, Antiplatelet therapy
Acute coronary syndrome (ACS) is a medical emergency and requires immediate hospital admission. ACS is the most prevalent cardiac disorder.1 It is a major cause of death and disability. The incidence of ACS is increasing day by day, because modification of life style and habit. There are many factors to develop ACS. Without modification of these factors or improvement in primary prevention and treatment, ACS remains the chief causes of death in most developed countries.2 Diseases of the coronary arteries are almost always due to atheroma and its complications, particularly thrombosis. The culprit lesion is usually a complex ulcerated or fissured atheromatous plaque with adherent platelet-rich thrombus and local coronary artery spasm. The thrombus may undergo spontaneous lyses over the course of the next few days, although by this time irreversible myocardial damage might occur. Most patients present when it is still possible to salvage myocardium and improve out.3
Platelets have a major role in the pathogenesis of ACS, where plaque rupture is followed by platelet activation and thrombus formation.4 When platelets are activated they become larger in size, which can be measured by both larger mean platelet volume (MPV) and platelet distribution width (PDW).5 Larger and hyperactive platelets play a pivotal role in accelerating the formation and propagation of intracoronary thrombus, leading to occurrence of acute thrombotic events.6 These observations have made the hypothesis that increased MPV and PDW are an index of platelet size that correlates with a reliable indicator of platelet activation. This indicator may also be potentially useful marker in cardiovascular risk stratification.7
Diagnosis of ACS is still a challenge despite the remarkable improvement in the diagnostic modalities. The criteria for diagnosis of ACS are clinical presentation, biochemical markers of acute ischemic injury and electrocardiographic (ECG) findings.8 Most of these events are clinically unrecognizable and biochemically undetectable until the onset of necrosis. In addition, the sensitivity of necrosis marker is time-dependent and even the highly sensitive and specific markers often give false-negative results on admission. ECG change occurs only after infarction; not in all chest pain.9 Although the troponin has greater diagnostic sensitivity, but they did not resolve the problem of early diagnosis. Because of slow release kinetics from damaged myocardium; and often unsuitable for early diagnosis because, 40-60% of acute coronary syndrome patients present with non diagnostic concentration of Troponin. The CK-MB (6-8 hrs after onset) has the diagnostic accuracy and quantification of myocardial necrosis. But CK-MB is not ideal for early risk stratification. So, it could say, the present cardiac markers are not sufficiently sensitive in early stage of ACS.That′s why an early and reliable marker is needed for accurate diagnosis of ACS when patients will attend in cardiac emergency department. This could lower the morbidity and mortality rates.
Platelet parameters especially MPV and PDW could be an important and reliable marker in early detection of ACS when other markers are not available.10 They can give the idea of variation of size and shape which passively reflect the platelet activation and platelet activation which is the main steps of ACS. Platelet parameters are easily obtained routinely with complete blood count (CBC) in fully automated hematology analyzer without any extra cost, time and extra sample. An increased PDW indicate more variation of platelet size and also may be the predictor of platelet turnover and functional status. Increased MPV indicates the platelet activity. PDW is more sensitive and specific than MPV.11 Early diagnosis of ACS can minimize its complication. MPV and PDW are better, cheaper test in contrast to CK-MB and Troponin can rapidly detect the ACS in early stage when patient attaining in the emergency department. MPV and PDW are used as diagnostic tools to exclude chest pain from non cardiac origin and are considered as sensitive and useful test along with other conventional cardiac biomarkers. So, the study was designed to identify the association of platelet parameters in acute coronary syndrome before and after anti-platelet therapy
This quasi experimental study was carried out in the Department of Clinical Pathology, in collaboration with the Departments of Cardiology, BSMMU and BIRDEM, Dhaka from September 2011 to August 2012. A total of 79 patients of aged 18 years and above) with clinically suspected ACS who were attended in cardiac emergency and admitted in coronary care unit (CCU) had been enrolled in this study (group I). Patients were enrolled according to history, clinical examination, ECG report, Troponin I positive or negative after cardiologist opinions. The study patients (group I) had angina or angina like chest pain, ECG changes (ST-elevation/ST-depression/T inversion/ appearance of Q wave), with or without troponin I positive and were treated with anti-platelet (e.g. Aspirin, clopidogrel- 300mg loading dose and 75mg daily). It was also observed the 63 control (group II) had angina like chest pain but normal ECG, negative troponin I and without antiplatelet therapy at outpatient department; those were diagnosed as chest pain other than cardiac origin. Some patients and controls were dropped out from the study due to subsequent follow-up. Consecutive sampling with set criteria was followed and interviewed face to face. All findings and information were documented in a pre designed data sheet with informed written consent. Known cases of patients with congenital heart disease, hepatic and renal impairment, and documented malignancy, previously treated with anti-platelet, anti-coagulants, anti-inflammatory, lipid lowering agents and traumatic chest pain were excluded from this study.
CBC with peripheral blood film (PBF) including platelet, ESR, platelet parameters (MPV and PDW), troponin I, serum creatinine, fasting blood glucose, lipid profile, SGPT were done for case selection. Angiogram was not done due to unavailable facility. About 5.0 ml blood was collected from each patient before antiplatelet therapy through an aseptic venipuncture from anticubital vein. From these 2.0 ml of that blood was collected in EDTA tube for CBC and PBF. 3.0 ml blood was transferred into a clean, dry test tube and was centrifuged within an hour of collection to separate the clear serum. After 5 days later 2.0 ml blood was collected from each patient after antiplatelet and anticoagulant therapy in cases and 2.0ml blood from control for CBC and PBF. CBC and platelet parameters were estimated by automated haematology autoanalyser (SYSMEX-XT 4000i) within 2 hours, which were again rechecked manually.
Prior to the commencement of this study, the research protocol was approved by the Institutional Review Board (IRB) of BSMMU, Dhaka. Data were processed and analysed using computer software statistical package for social sciences (SPSS version 17). The test statistics were used to analyse the data including mean±standard deviation (SD), t-test, and Chi-square test with 95% confidence interval. Test of validity done by receiver operative characteristic (ROC) analysis curves.
A total of 142 patients were included in this study. Some forty two percent patients age belonged to 51-60 years with mean age 55.05±10.73(31-80) years in group I and 22(34.9%) patients age belonged to 41-50 years with mean age 48.4±10.39(28-70) years in group II. Male was predominant in both groups, 57(72.2%) in group I, and 44 (69.8%) in group II. The male: female was about 2.3:1 in both groups. Regarding the baseline characteristics of the study patients, in CBC parameters, only mean neutrophil percentage and ESR difference was statistically significant (p<0.05) but WBC count was not statistically significant (p>0.05) between the groups. Triglyceride, total cholesterol and LDL cholesterol was statistically significant (p=0.001) but HDL cholesterol was not statistically significant (p= 0.668). Troponin I was found positive in 53(67.1%) patients in group I but none in group II. The difference was statistically significant (p<0.05) between the groups.
| Variables |
Group I |
Group II |
p |
||
|---|---|---|---|---|---|
|
Mean |
±SD |
Mean |
±SD |
|
Plateletcount (109/L) |
|
|
|
|
|
Before (1st sample) |
273.1 |
±50.15 |
290.78 |
±74.86 |
0.096 |
Range (min-max) |
(190 |
-450) |
(150- |
610) |
|
After (2nd sample) |
284.56 |
±41.93 |
323.7 |
±69.2 |
0.001 |
Range (min-max) |
(150 |
-450) |
(150 |
-500) |
|
p value |
0.052ns |
0.058ns |
|
||
MPV (fI) |
|
|
|
|
|
Before (1st sample) |
12.48 |
±1.17 |
10.45 |
±0.66 |
0.001 |
Range (min-max) |
(9.20 |
-16.2) |
(9.1 |
-12.5) |
|
After (2nd sample) |
11.55 |
±1.08 |
10.17 |
±0.76 |
0.001 |
Range (min-max) |
(9.1 |
-14) |
(8.6 |
-11.9) |
|
p value |
0.001s |
|
|
||
PDW (fI) |
|
|
|
|
|
Before (1st sample) |
16.23 |
±2.56 |
11.89 |
±1.42 |
0.001 |
Range (min-max) |
(10.1 |
-25.6) |
(9.7 |
-16.5) |
|
After (2nd sample) |
14.29 |
±2.11 |
11.49 |
±1.39 |
0.001 |
Range (min-max) |
(9.5 |
-19.2) |
(8.9 |
-14.9) |
|
p value |
0.001s |
||||
In ECG findings, myocardial infarction was found 67(84.8%) patients, and UA in 12(15.2%) patients in group I and all ECG was found normal in group II (100.0% cases). The difference was statistically significant (p<0.05) between the groups (table I).
The mean (±SD) platelet parameter showed in table-I before (1st sample) and after (2nd sample) anti-platelet therapy in group I, and subjects in group II mean (±SD) platelet parameter between 1st and 2nd samples. In 1st sample the mean (±SD) platelet count was 273.1(±50.15) 109/L and 290.78(±74.86) 109/L in group I and group II respectively and there was no statistical significance found between the groups (p =0.096). In 2nd sample the mean (±SD) platelet count was 284.56(±41.93) 109/L in group I and 323.57(±69.2) 109/L in group II and there was statistical significant differences found between the groups (p =0.001). In-group I, 1st and 2nd samples, the mean platelet count differences was not statistically significant (p =0.052). Both 1st and 2nd samples, the mean (±SD) MPV was 12.48(±1.17) fl and 11.55(±1.08) fl in group I and it shows statistically significant differences (p =0.001). In-group II, MPV was 10.45(±0.66) fl in 1st sample and 10.17(±0.76) fl in 2nd sample respectively. Comparison of 1st sample in both groups the MPV differences was statistically significant (p<0.05).
|
Cut of value |
Sensitivity (%) |
Specificity (%) |
Accuracy (%) |
PPV (%) |
NPV (%) |
Area undee |
95% Confidence interval (CI) |
|
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
ROC ce |
Lower |
Upper |
Platelet |
>225) |
83.0 |
28.1 |
42.3 |
37.6 |
64.0 |
0.428 |
0.333 |
0.524 |
MPV |
>10.7) |
90.6 |
49.4 |
64.8 |
51.6 |
89.8 |
0.824 |
0.754 |
0.895 |
PDW |
>12.7) |
94.3 |
52.8 |
69.0 |
54.9 |
94.1 |
0.846 |
0.780 |
0.912 |
In 1st sample, the mean (±SD) PDW was 16.23(±2.56) fl and 11.89(±1.42) fl in group I and group II respectively and these were statistically significant (p=0.001). In 2nd sample, the mean (±SD) PDW was 14.29(±2.11) fl in group I and.11.49(±1.39) fl in group II and these were also statistically significant (p=0.001). In-group I, the mean PDW difference was statistically significant (p<0.05) between the samples (table II).
Receiver-operator characteristic (ROC) curves of platelet count, MPV and PDW for prediction of ACS. The area under the receiver-operator characteristic (ROC) curves for the ACS predictors by troponin I is depicted in table II. Based on the receiver-operator characteristic (ROC) curves PDW had the best area under curve compared to platelet counts and MPV. ROC were constructed using PDW value of the patients between two groups, which gave a PDW cut off value of >12.7 fl as the value with a best combination of sensitivity and specificity for ACS. At this PDW cut-off value of >12.7 fl, the sensitivity and specificity of PDW in diagnosing acute coronary syndrome was found94.3% and 52.8%, respectively (figure 1).
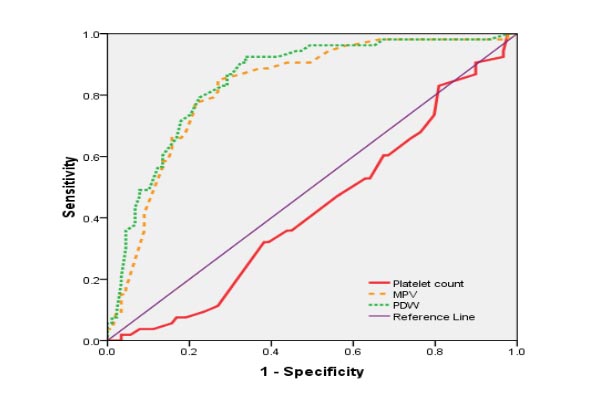
Platelet count cut-off value of >225X109/L showed sensitivity 83.0% and specificity 28.1% in the diagnosis of acute coronary syndrome. MPV cut-off value of >10.7 fl showed sensitivity 90.6% and specificity 49.4% in the diagnosis of acute coronary syndrome. Accuracy, positive predictive values and negative predictive values are shown in the table II.
Discussion
In this study, it was to be found that ACS was associated with abnormal platelet parameters. The study reveals that the mean (±SD) value of total platelet count was lower in cases than controls. Whereas MPV and PDW were significantly higher in group I than group II. Similar findings were to be found in some other studies.11-13Platelet volume is an important indicator for platelet function and activation. There are many studies done where platelet volume associated with ACS. Varol et al andYilmaz et al also found that MPV was significantly higher in patients with ACS groups than controls, along with reverse changes in platelet count.14,15 Similar findings were to be found study done by Pizzuli et al and Mercan et al.16,5 They found platelet counts were significantly lower in the ACS groups as compared to control subjects, but MPV was significantly higher in ACS. Independent association of MPV in AMI had shown Endler et al.4 They also showed the higher the MPV the higher is the risk of MI. Park et al considered increased MPV to be a risk factor for platelet activation.17 Yasar et al observed in their studies, increased MPV on admission predicts impaired reperfusion, where there is activation of platelet before AMI begins, and consequently, there are more death occur in those patients after thrombolytic therapy.18 The MPV remain increased up to 5/6 days suggest that the activity of platelets remain constant. Chu et al found that MPV was associated with patients AMI and described MPV as a risk factor and prognostic indicator in cardiovascular disease.19 Lippi et al were found in their study MPV was significantly associated with ACS than with non-ACS.4
So far, there were only two studies found on values of platelet count and PDW as known to us. But in Bangladesh, so far, there were no study found on platelet parameters and ACS. Here, with the findings of platelet count and PDW sensitivity and specificity in this study will enrich diagnostic modalities in patients with ACS. The sensitivity, specificity, positive and negative predictive values were determined through ROC curves against troponin I positive. In our study among the 79 cases, 53 were troponin I positive and 26 were troponin I negative. All of the control subjects were troponin I negative. According to the diagnostic criteria, 67 cases were diagnosed as AMI and 12 cases were UA, where troponin I was negative. Among 67 AMI cases, only 53 cases were troponin I positive in 1stsample and 14 cases were initially negative troponin I and became positive later. That is why specificity was low in this study because there was similar result of platelet parameters found in troponin I positive and negative subjects in group I.
In the present study, total counts of platelet are in group I before and after anti-platelet therapy were denoted no significant differences between the samples. In case of MPV and PDW, it was found that the significant differences before and after anti-platelet therapy, but not below the cut off values. These suggest that MPV and PDW are indirect indicators of platelet activation and their association with ACS. After anti-platelet therapy, MPV and PDW were decreased, due to inhibition of platelet activation and aggregation. Among the platelet parameters, PDW was most significant than MPV. These findings lead to the hypothesis that larger platelets as determined by their volumes, MPV and PDW may be useful markers in patients with ACS. Data indicate that, higher MPV and PDW may become useful marker for early detection of ACS along with other biomarkers.
Conclusion
Larger platelets are haemostatically more active and a risk factor for developing coronary thrombosis leading to ACS. Patients with increased MPV and PDW, which could be easily identified during routine haematological analysis. It could play an important role in early detection of ACS and early initiation of anti-platelet therapy and thereby prevention and development of full-blown of ACS. It could be used as a screening test to differentiate the origin of chest pain along with other cardiac biomarkers. It is also used to assess outcome of ACS and AMI which needs to be monitored.
Acknowledgments
We acknowledge with gratitude to all patients whose participation made this study possible. We also express special thanks to some specialists, nurses and other staffs in the Departments of Clinical Pathology and Cardiology of BSMMU and BIRDEM, Dhaka.
References
- Pollack CV Jr, Antman EM, Hollander JE. 2007 focused update to the ACC/AHA guidelines for the management of patients with ST-segment elevation myocardial infarction: implications for emergency department practice. American College of Cardiology; American Heart Association. Ann Emerg Med. 2008; 52: 344-355.
- Assiri AS, Jamil AM, Mahfouz AA, Mahmoud ZS, Ghallab M. Diagnostic importance of platelet parameters in patients with acute coronary syndrome admitted to a tertiary care hospital in southwest region, Saudi Arabia. J Saudi Heart Assoc. 2012; 24:17-21.
- Lippi G, Filippozzi L, Salvagno GL, et al. Increased mean platelet volume in patients with acute coronary syndromes. Arch Pathol Lab Med. 2009; 133:1441-3.
- Endler G, Klimesch A, Sunder-Plassmann H, et al. Mean platelet volume is an independent risk factor for myocardial infarction but not for coronary artery disease. Br J Haematol. 2002; 117:399-404.
- Mercan R, Demir C, Dilek I, Asker M, Atmaca M. Mean platelet volume in acute coronary syndrome. Van Tip Derg. 2010; 17:89-95.
- Martin JF, Bath PM, Burr ML. Influence of platelet size on outcome after myocardial infarction. Lancet. 1991; 338:1409-1411.
- Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined - a consensus document of the joint European Society of Cardiology/ American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000; 36:959-969.
- Richard B. Emergent diagnosis of acute coronary syndromes: Today’s challenges and tomorrow’s possibilities. Resuscitation. 2008; 78:13-20.
- Chu Hsin, Chen WL, Huang CC, Chang HY, Kuo HY, Gau CM, Chang YC, Shen YS. Diagnostic performance of mean platelet volume for patients with acute coronary syndrome visiting an emergency department with acute chest pain: the Chinese scenario. Emerg Med J. 2011; 28: 569-574.
- Vagdatli E, Gounari E, Lazaridou E, Katsibourlia E, Tsikopoulou 3, Labrianou I. Platelet distribution width: a simple, practical and specific marker of activation of coagulation. HIPPOKRATIA. 2010; 14:28-32.
- Mathur A, Robinson MSC, Cotton J, Martin JF, Erusalimsky JD. Platelet Reactivity in Acute Coronary Syndromes: Evidencefor Differences in Platelet Behaviour between Unstable Anginaand Myocardial Infarction. Thromb Haemost. 2001; 85:989-994.
- Nandwani S, Bhatnagar M, Gaur S, Kumar M. Study of Platelet Volume Indices in Patients of Acute Coronary Events. Journal of the Indian Academy of Geriatrics. 2011; 7: 22-24.
- Khandekar MM, Khurana AS, Deshmukh SD, Kakrani AL, Katdare AD, Inamdar AK. Platelet volume indices in patients with coronary artery disease and acute myocardial infarction: an Indian scenario. J ClinPathol. 2006; 59: 146-9.
- Varol E, Icli A, Ozaydin M, Erdogan D &Arslan A. Mean platelet volume is elevated in patients with myocardial infarction with normal coronary arteries, as in patients with myocardial infarction with obstructive coronary artery disease. Scandinavian Journal of Clinical & Laboratory Investigation. 2009; 69570-574.
- Yilmaz MB, Cihan G, Guray Y, Guray U, Halil LK, Sasmaz H, Korkmaz S. Role of mean platelet volume in triagging acute coronary Syndromes. J Thromb Thrombolysis. 2008; 26: 49-54.
- Pizzulli L, Yang A, Martin J.F. and deritz BL. Changes in platelet size and count in unstable angina compared to stable angina or non-cardiac chest pain. European Heart Journal. 1998;19:80-84.
- Park Y, Schoene N, Harris W. Mean platelet volume as an indicator of platelet activation: methodological issues. Platelets. 2002; 13: 301-306.
- Yasar AS, Bilen E, Yuksel IO, Arslantas U, Karakas F, Kirbas O, Bilge M. Association between admission mean platelet volume and coronary patency after thrombolytic therapy for acute myocardial infarction. TurkKardiyol DernArs - Arch Turk Soc Cardiol. 2010; 3885-89.
- Chu SG, Becker R C, Berger P B, Bhatt D L, Eikelboom JW, Konkle B, Mohler E R, Reilly MP and Berger JS. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. Journal of Thrombosis and Haemostasis. 2010; 8: 148-156.